For 10 months, I had the opportunity to be a Patient Care Associate (or nurse’s aid) with Norton Healthcare in Louisville, Kentucky. When I applied for the job, I expected not to get it because at that point I had only volunteered with hospice and had no hands-on experience. To my surprise, I was happily accepted (probably because healthcare is short-staffed). However, they placed me into a unit that was the best fit for me, a Neurological Progressive Care Unit. As a neuroscience major, of course, I was excited to see firsthand the stuff I read about in books. Here, I will share 5 take-aways that nursing staff (especially PCA’s) may implement in their care to maximize both the patient’s and your own experience. The things I share here of course are my own philosophy: I’m in no way perfect and have many areas of improvement, and still have bad days. Nonetheless, these habits are always dependent on nurse and aid to patient ratios, and it is my hope that you practice these habits when time allows.
1. If a patient can stand-pivot to a chair, then they can stand-pivot into the shower.
Whenever we think of the ‘philosophy’ behind being a step-down or PCU, we should implement progressive goals for our patients to get them near their baseline. Bed baths have their place for sure, but nothing puts a smile on a patient’s face and gives them the confidence they need than getting them in the shower. It’s okay to get creative with patient care, so long as the nurse’s are on board. I usually will take either a wheelchair, or a recliner, push it into the bathroom, and pivot that patient into the shower. It really makes a world of difference and allows them to set new standards for themselves. Much of a patient’s plan of care is them believing and having confidence in themselves to get well (think reducing cortisol levels, placebo effect, unofficial PCA-assisted physical/occupation therapy, etc.)
2. Play music when appropriate.
You can be surprised by how much you can connect with a patient through music. One of my favorite memories as a PCA was meeting other Christians. There are 2 situations where talking to other Christians came up naturally. First, families really appreciate it when you give their patients a shower. Many times, they will ask about your goals, personal life, and take an interest in why you are providing excellent progressive patient care. Secondly, is music. In all my baths/showers, I will ask a patient what their favorite music/artist is. At one point, I had a patient request Lauren Daigle, an artist that I also loved, and we sang/worshiped Jesus together while I helped her with her bath. Only Jesus is able to make a vulnerable, sometimes awkward situation turn into something beautiful. Music also uplifts you, because working in healthcare is hard. So, play music when appropriate.
3. Open the blinds.
Such a small thing, and we even chart in our safety rounds “Appropriate illumination of the room.” In an effort to reduce hospital delirium, disorientation, and to regulate the patient’s circadian rhythm, open the blinds. The circadian rhythm is a natural internal process that helps the sleep-wake cycle; plus, our patients need their Vitamin D. We do not want our patients sleeping during the day because that is when physical/occupation therapy sessions happen, doctors round, and family visits. We do not want the patient to be lethargic and miss out on those opportunities to feel supported by loved ones, educated, and have a voice in their plan of care.
4. Don’t apologize for not knowing or situations out of your control.
When you’re working in healthcare, you are constantly learning. Whether that is from physicians, nurses, supply techs, PCA’s, etc. That is what’s beautiful about the practice of medicine. Nobody should expect you to know everything, and they probably don’t. So don’t be so hard on yourself. When you learn something new, respectfully thank that person for teaching or showing you a different perspective, method, or policy. Thanking them conveys a spirit of receptiveness to learning more. When you apologize, you may communicate that you are unapproachable or nonreceptive to learning. I like to bypass all of that and periodically give the nurses an opportunity to explicitly share with me areas I can improve; you’ll be so thankful for the conversations, and so will your nurses. As always, 7% of meaning is communicated through spoken word, 38% through tone of voice, and 55% through body language.
5. Be human and keep learning.
There are many tips and tricks that I can teach, but to be honest, most of these daily habits come from the heart of caring about other nurses and the patients. Even some if not all of the aforementioned habits. It’s something that can’t really be taught, only internalized. For example:
Stealing draw sheets from the ICU make it easier for me and the nurses to reposition patients, maximizing their comfort and keeping our backs safe; cleaning patient rooms gives a patient a sense of organization in their temporary home, and allows rapid or code blues to have maximum staff and equipment to fix the problem; offering help to nurses and aids, even when it’s not on my patient, creates a culture of servitude on the unit, something we could all benefit from, but it starts with me; giving objective reports, staying away from subjective and opinion, so that the nurse/aid taking care of the patient offers the maximum quality of care and form their own opinion; learning how to maximize the use of the Epic system software provides more accurate information and care. And so on, so on, so on.
Most, if not all the things listed here, one doesn’t “have” to do. All you can do is control your own actions and attitude, and so long as that patient has you for the day, maximize their experience so that at the end of the day, when you give bedside report, few of them will thank you with their warm smiles and handshakes (sometimes hugs), and help you remember why you do what you do. Each patient is unique, and you have to find what that “little” thing is for each of them that will make their day. You’ll find that when your patients love you for the little things, it is much easier to love your career. Let you be the best thing that’s happened to them during their stay, and believe that you are.
Nurses, thank you for all that you do. I will leave you with one of my favorite quotes:
“Through my training and career, nurses have been my hands, my eyes, and my ears. They have caught my sleep-addled mistakes at 3 a.m. when I was an exhausted house officer. They’ve been valuable members of our team and advocates for our patients. Every time I have run to a bedside to help save a life, it was because the nurse called me there. I remember being sent on the NICU transport from another hospital; I was also terrified I wouldn’t know what to do if something went wrong but I had an experienced nurse with me. She knew what to do.
Do you know why I’m a physician and not a nurse? Because I’m not brave enough to be a nurse.
So for all the nurses out there, I stand with you.”
-Mike Ginsberg, MD.
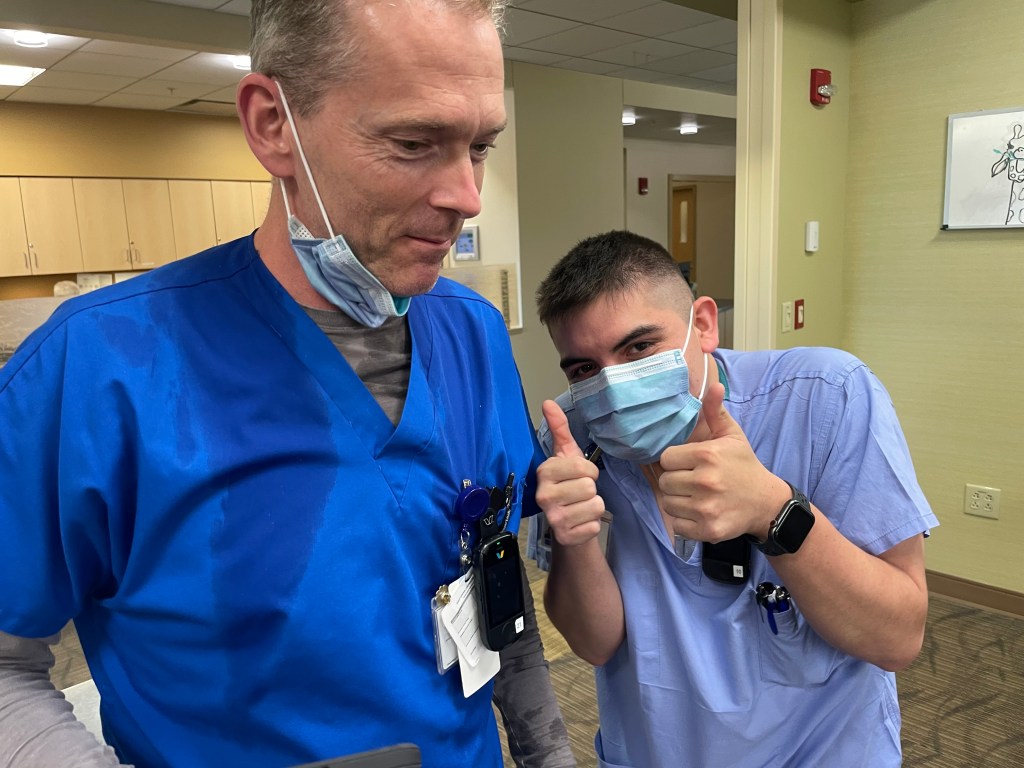
To my 3/4 West Neuro staff, thank you so much for pouring into this future physician, and dealing with my saline flush attacks, snowball fights, 6/10 haircuts, the tough days, and most of all my personality. You all are heroes and will always have a place in my heart. I will be a better physician because of each of you. Please stay in touch.
Okay Vocera, Log Out.
-Ricardo